Learn about the diagnostic and operative hysteroscopy procedure at Usha IVF. Expert insights, advanced techniques, and compassionate care for optimal outcomes.
Usha IVF, located in Anand, Gujarat, offers advanced diagnostic and operative hysteroscopy procedures to address a range of gynecological concerns. Our highly skilled and experienced team of doctors specializes in hysteroscopy, a minimally invasive procedure that allows for thorough evaluation and treatment of the uterus.
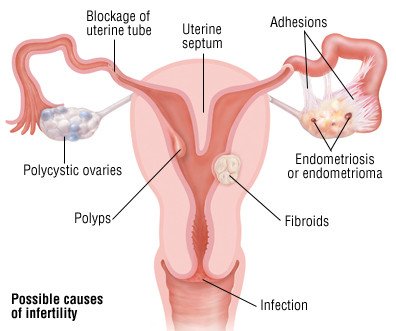
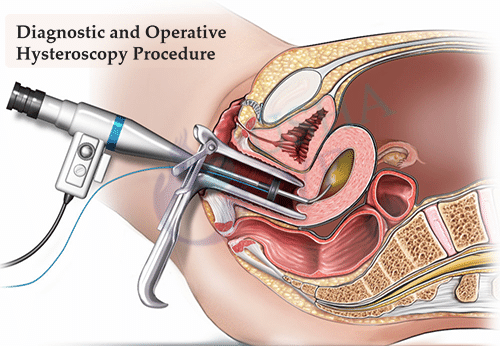
A Diagnostic and Operative Hysteroscopy Procedure is useful in identifying sources of abnormal uterine bleeding and dysmenorrhea, such as fibroids, adhesions, and polyps. It is also used to further evaluate abnormalities and is renowned for firm diagnostic tests such as a hysterosalpingogram, sonogram, or endometrial biopsy. Surgical procedures to correct some Diagnostic and Operative Hysteroscopy problems can be carried out with operative hysteroscopy, using special instruments that fit complete the channels of the hysteroscope.
A hysteroscope is a long, slight telescopic device that is used to view the inside of the uterus. It is used not only to diagnose such situations as fibroids, holds, and polyps (diagnostic) but also to treat them (operative hysteroscopy). Instruments designed to fit through a channel in the hysteroscope are used to remove growths or scar tissue or to correct certain inherited aberrations such as a uterine septum. Because the uterine cavity is a possible one, it must be overstated with either a harmless gas or fluid to make space for viewing and operating. This can cause constrictions similar to menstrual cramps. Afterward, depending on the procedure performed, there may be vaginal release or bleeding for several days.
Hysteroscopy
The purpose of a hysteroscopy is to diagnose and treat abnormal bleeding by looking inside the uterus. A hysteroscopy is a procedure that uses a thin, lighted tube to examine the cervix and the inside of your uterus via the vaginal canal. Operative hysteroscopy can be used to remove growths, fibroids, and holds.
At Usha IVF, we prioritize patient comfort and safety. Our team is dedicated to providing personalized care and ensuring a supportive environment throughout the hysteroscopy procedure. We understand that each patient’s needs are unique, and we take the time to listen, explain the procedure, and address any concerns.
If you require diagnostic or operative hysteroscopy, trust the expertise of Usha IVF. Our skilled team, state-of-the-art facilities, and patient-centered approach make us a leading choice for hysteroscopy procedures.
Frequently Asked Questions: Diagnostic and Operative Hysteroscopy Procedure at Usha IVF
Q: What is hysteroscopy?
⇒ Ans: Hysteroscopy is a medical technique in which the interior of the uterus (womb) is examined using a thin, illuminated device called a hysteroscope. It can be done as a diagnostic technique to look into certain gynecological issues or as an operational treatment to address specific uterine anomalies.
Q: Is a Diagnostic and Operative Hysteroscopy Procedure necessary for me?
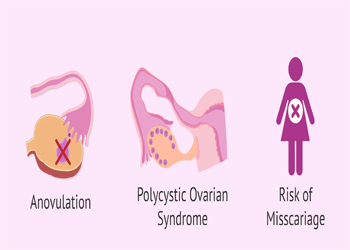
⇒ Ans: If you have abnormal uterine bleeding, recurrent miscarriages, infertility, or other uterine or cervical concerns, a Diagnostic and Operative Hysteroscopy Procedure may be indicated. It enables the clinician to examine the uterine cavity visually, diagnose abnormalities such as polyps, fibroids, adhesions, or structural problems, and take tissue samples for future study.
Q: What exactly is an operational hysteroscopy?
⇒ Ans: Operative hysteroscopy is a treatment that not only allows the doctor to see the uterus cavity but also allows the doctor to execute surgical operations to cure specific uterine diseases. Polyps, fibroids, adhesions, and the uterine septum can all be removed with it. It can also be used for endometrial ablation or the removal of intrauterine devices (IUDs) that have become trapped in the uterus.
Q: How does a hysteroscopy work?
⇒ Ans: A hysteroscopy is often conducted as an outpatient procedure. A hysteroscope is inserted via the vagina and cervix into the uterus during the operation. To improve visualization, carbon dioxide gas or a saline solution may be used to widen the uterine cavity. The hysteroscope sends pictures to a monitor, allowing the clinician to check the uterine lining or perform surgical treatments as needed.
Q: Does hysteroscopy hurt?
⇒ Ans: Hysteroscopy is usually easily tolerated and generates little pain. To numb the cervix and lessen any possible pain, local or general anesthesia may be utilized. Following the surgery, some individuals may have moderate cramping or vaginal spotting, although these symptoms normally pass rapidly.
Q: What are the prerequisites for hysteroscopy?
⇒ Ans: Your doctor will give you precise instructions, although you may be requested to refrain from sexual activity, vaginal drugs, tampons, or douching for a few days before the operation. It’s critical to tell your doctor about any drugs you’re taking, since some, such as blood thinners, may need to be changed before the treatment.
Q: What are the risks and consequences of hysteroscopy?
⇒ Ans: Hysteroscopy is usually thought to be safe. However, like with any medical operation, there are hazards, such as infection, hemorrhage, uterine or cervix injury, and anesthesia response. These hazards are uncommon, and your doctor will take the appropriate efforts to reduce them.
Q: How long does it take to complete the procedure?
⇒ Ans: The length of a Diagnostic and Operative Hysteroscopy Procedure varies according to the procedure’s goal and any further treatments necessary. Depending on the intricacy of the procedure, diagnostic hysteroscopy may take 15 to 30 minutes, whereas operative hysteroscopy may take somewhat longer.
Q: How long does it take to recuperate after a hysteroscopy?
⇒ Ans: Hysteroscopy is often conducted as an outpatient procedure, allowing you to return home the same day. For a day or two after the surgery, you may suffer minor cramping or vaginal spotting. Most women may return to their typical activities after a day or two, but it’s critical to follow your doctor’s advice on any limits on physical activity, bathing, or other activities.