Low AMH and Guidance for Pregnancy | Low AMH: Understanding the Impact on Fertility and Strategies for Pregnancy
From personalized treatment plans, including IVF and egg donation, to emotional support, Usha IVF provides low AMH and guidance for pregnancy with the tools and resources you need to overcome low AMH and achieve your dream of starting a family. Don’t let low AMH hold you back from becoming a parent. Contact us today with Usha Ivf center in Anand to schedule a consultation with you and take the first step towards parenthood. Low AMH (anti-Mullerian hormone) can be a challenging diagnosis for people and couples trying to create. This article provides an overview of what low AMH means, its effect on fertility, and guidance on strategies for gaining pregnancy.
Methods for naturally increasing AMH levels
It is possible to naturally increase your AMH levels. Eating a diet high in essential nutrients, such as vitamin D, can help your body naturally increase levels of AMH. Additionally, studies have shown that women who took the micronutrients in Impryl had elevated levels of AMH.
AMH: What is it? | What exactly is AMH?
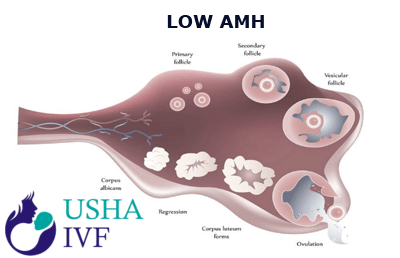
Despite being made in both male and female reproductive organs, AMH is typically only detected in females. This is due to AMH being produced by the follicles growing in a woman’s ovaries. The fundamental idea is that your AMH levels rise and vice versa as your egg count increases. In order to assess ovarian reserve and help clinics prepare for your treatments and medications, AMH levels are evaluated prior to IVF. AMH levels are a crucial indicator of the amount of eggs still present, but they are not a reliable predictor of the quality of the eggs being produced, it is vital to keep in mind.
Why is my AMH low?
Despite being made in both male and female reproductive organs, AMH is typically only detected in females. This is due to AMH being produced by the follicles growing in a woman’s ovaries. The fundamental idea is that your AMH levels rise and vice versa as your egg count increases. In order to assess ovarian reserve and help clinics prepare for your treatments and medications, AMH levels are evaluated prior to IVF. AMH levels are a crucial indicator of the amount of eggs still present, but they are not a reliable predictor of the quality of the eggs being produced, it is vital to keep in mind.
Levels of AMH and Fertility
The term Anti-Müllerian Hormone (AMH) levels may be familiar to you if you have ever considered getting a fertility MOT. Your ovarian reserve will be evaluated by a fertility MOT that counts the antral follicles (AFC) or measures AMH.
What do AMH levels signify for you and what are they?
Ovarian follicles that are growing egg sacs release AMH. The amount of AMH in your bloodstream increases as more eggs are still present in the ovaries. Therefore, it is believed that a low amount of AMH indicates a low ovarian reserve (a low number of developing egg sacs). It’s typical for a woman who is getting close to menopause to have low levels of AMH.
AMH levels between 1.0 and 3.0 ng/mL are regarded as “normal.” AMH levels below 1.05 ng/ml are regarded as very low, while those below 0.16 ng/ml are referred to be “undetectably low.”
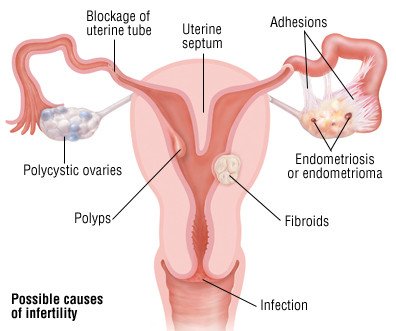
A low AMH may result from various factors, such as
- Your age – AMH levels will normally decrease as you age.
- Surgery for ovarian cysts or endometriosis
- An Autoimmune Disease
- You’re DNA
Analyzing AMH test outcomes
The number of eggs still in a woman’s ovarian reserve can be determined by an AMH test. AMH levels between 1.0 and 3.0 ng/mL are regarded as “normal.” AMH levels below 0.16 ng/ml are referred to as “undetectably low” AMH levels, and AMH levels below 0.9 ng/ml are termed low AMH. Different AMH levels can signify various reproductive problems in women.
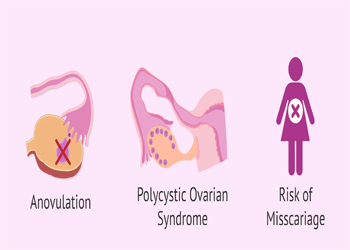
AMH levels naturally decline with age, but if they are very low for your age, it may be a sign of impending menopause. AMH levels that are extremely high may signal polycystic ovary syndrome (PCOS). Your test findings will reveal how many eggs you still have, but not their quality or state of health.
How might AMH levels normally rise?
It is generally known that a decline in AMH levels with advancing age indicates low ovarian reserve as the menopause draws near. AMH levels can naturally fall from one cycle to the next, but they can also naturally rise, and this does not necessarily follow what seems to be a traceable pattern. This is because it is normal for AMH levels to fluctuate from one cycle to the next. A diet high in essential minerals, such as vitamin D, can help your body naturally elevate levels of AMH, even if it may be difficult to forecast whether you will experience months with a greater or lower AMH level.
Fertility with Low AMH Levels
The good news is that although while low AMH indicates that your ovarian reserve is low, it does not exclude you from becoming pregnant naturally. With low AMH, it is entirely possible to become pregnant using either your own or donor eggs. After all, all it takes is one sound egg.
There are other ways to increase your fertility besides increasing your AMH level, thus it won’t fully convey your fertility tale. Depending on your specific circumstances, you might be encouraged to attempt IVF if you’re having trouble. If the levels drop too low, your chances of getting pregnant naturally may be reduced, but you can still talk to your doctor about all your choices.
What does having low AMH levels signify for my IVF success rates?
Here are some things for you to think about if you decide to undergo IVF after having trouble becoming pregnant. First off, you shouldn’t worry too much if your AMH levels are low but quantifiable if you are younger, which is generally regarded to be below the age of 35 in the field of fertility. You will be given medicine that will encourage your body to generate follicles, which given your age are likely to be of high quality. Keep in mind that low AMH does not indicate bad-quality eggs, but rather lesser quantity, which is less significant when using assisted reproductive technologies (ART).
In conclusion, our study suggests that significantly diminished AMH or the Anti-Mullerian Hormone is associated with an increased risk of miscarriage in spontaneously developed pregnancies. While AMH may not be an independent quality of fecundability, low AMH or diminished ovarian fund may be a marker of reduced reproductive potential due to its association with pregnancy failure. Further analysis is needed to identify the biological tool underlying this relationship.